Federal authorities are turning up the heat even more in their battle against Medicare home health fraud. The top targets: More than 500 home health agencies and 4,500 physicians identified as having suspicious practices as compared with most providers nationally.
To identify these providers, the Office of Inspector General (OIG) for the Department of Health and Human Services did some data analysis. After analyzing recent home health frauds, the OIG pulled out five common characteristics in these cases:
1. High percentage of episodes for which the beneficiary had no recent visits with the supervising physician
2. High percentage of episodes that were not preceded by a hospital or nursing home stay
3. High percentage of episodes with a primary diagnosis of diabetes or hypertension
4. High percentage of beneficiaries with claims from multiple HHAs
5. High percentage of beneficiaries with multiple home health readmissions in a short period of time
About 5% of all HHAs and 1% of all physicians who supervise home health care are statistical outliers on two or more of these characteristics, the OIG determined. That translates to 526 HHAs and 4,502 doctors.
Just because these providers are outside the norm in terms of their claims data does not mean they are perpetrating fraud, the government watchdog acknowledged in a data brief issued Wednesday. However, OIG is planning to conduct investigations and audits of these providers and/or refer them for followup by the Centers for Medicare & Medicaid Services (CMS).
The agency did not identify these providers by name in its public report.

Of the five warning signs of potential fraud, having a high percentage of readmissions shortly after discharge was most common among home health agencies. Nearly 780 agencies were outliers, meaning more than 19% of their patients fit this description, compared with a national median of 5.6%.
“Past OIG fraud investigations have uncovered incidents in which HHAs provided—and physicians supervised—unnecessary care over a long period of time and tried to conceal the duration of that care by periodically discharging and re-enrolling their beneficiaries,” the report authors wrote.
Collusion between physicians and home health agencies in several of these schemes is another area of particular concern to the OIG, which issued a separate alert on Tuesday detailing improper arrangements and conduct between these parties.
Fraud Zones
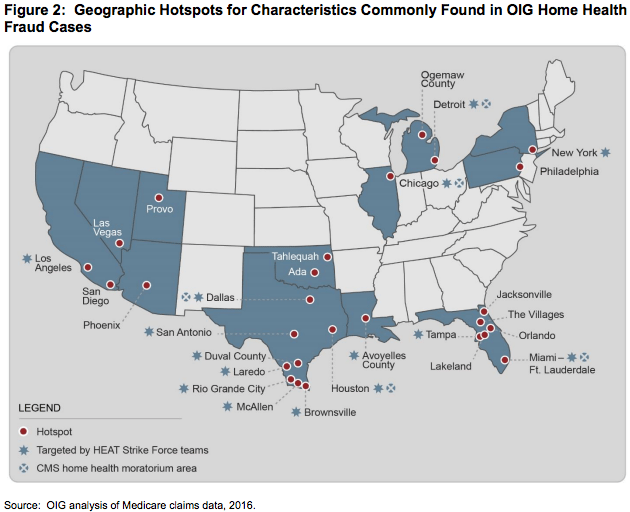
There are 27 “hotspots” in 12 states where suspicious activity is clustered, the OIG determined, by looking at criteria such as the concentration of HHAs that were outliers on two or more of the five characteristics of fraud.
Some of these are cities such as Miami, Chicago, and Houston that already are notorious for home health fraud—so much so that CMS has placed moratoria on certifying any new home health providers there.
But some of the newly identified hotspots have not been under such intense scrutiny, so providers in these areas might want to brace for more OIG activity. They include Las Vegas, San Diego, Phoenix, and Ada, Oklahoma.
Home health fraud continues to be rampant, and providers should expect the “fight” to continue in the form of investigations, audits, evaluations, and enforcement actions, the OIG emphasized in the conclusion of its data brief.
Reinforcing this message, several home health agencies were targeted in the largest-ever roundup of alleged Medicare fraudsters, announced Tuesday by the Department of Justice.
Written by Tim Mullaney




