Despite individual concerns and procedural roadblocks in some states, many home health and home care providers say their workers have been able to gain access to the available COVID-19 vaccines.
As the U.S. neared a large-scale vaccine rollout, some in-home care operators feared their clinicians and caregivers would be overlooked, especially with government officials often focused more so on hospital and nursing home staff. The fact that several states have explicitly recognized home care professionals as eligible for the COVID-19 vaccine is particularly encouraging, Darby Anderson, vice chairman of the Partnership for Medicaid Home-Based Care (PMHC), told Home Health Care News.
The Washington, D.C.-based PMHC is an industry advocacy group that represents home- and community-based care providers operating in the Medicaid space.
In addition to his role at PMHC, Anderson also serves as executive vice president and chief strategy officer for Addus HomeCare Corporation (Nasdaq: ADUS). Headquartered in Frisco, Texas, Addus provides personal care, home health and hospice services across nearly two dozen states.
“It’s maybe a little easier on the nursing, therapy and more clinical [roles], to have them acknowledged as health care workers needing the vaccine,” he said. “We had concerns initially that it would be harder for the home care aides and more paraprofessional staff to be considered in that health care group, but that honestly met very little resistance.”
To help gauge vaccination progress, HHCN recently polled more than 100 home-based care professionals. Roughly two-thirds of the respondents worked for Medicare-certified home health agencies, with the remainder working for Medicaid and private-pay in-home care providers.
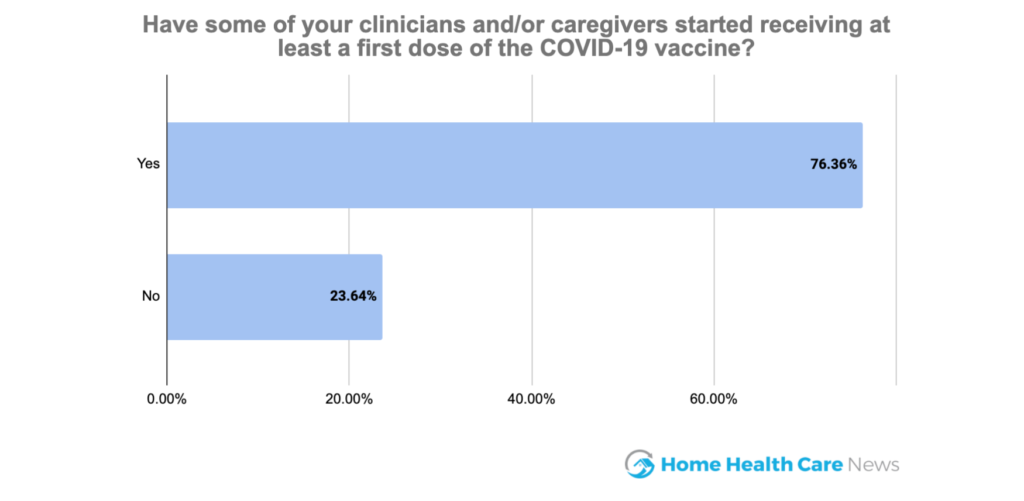
Overall, more than three-quarters of survey respondents said they have staff members who have received at least a first dose of the COVID-19 vaccine. Staff members have typically gotten their shots via external vaccination sites, though about 17% of the HHCN survey respondents reported their organizations are doing in-house vaccinations.
The Visiting Nurse Service of New York (VNSNY), for example, decided to internally handle staff vaccinations to speed up the process and maximize efficiency. So far, the nonprofit home-based care giant has vaccinated 2,000 of its eligible employees.
“Our staff [members] who want the vaccine are very [eager] to get it,” VNSNY Chief of Provider Services Andria Castellanos previously told HHCN. “As a large employer who really cares about our employees, we felt like we could deliver the vaccine to them faster than they could likely get it in the rest of the city.”
The ‘sausage-making process’
While the vaccination rollout to home health and home care workers appears to be going smoothly on the whole, there are still isolated problems due to mixed messages and confusing guidance.
Certain in-home care workers in Florida have claimed they’re not getting sufficient access to the COVID-19 vaccine, for instance, which goes against an executive order from Republican Gov. Ron DeSantis.
Specifically, the order states the first phase of vaccine distribution should include all health care personnel with “direct patient contact.” Yet some vaccine sites aren’t lumping home health or home care staff into that group.
“We are classified in the executive order; we are just not being recognized as such,” Shayna Adaniel, the director of client services for BrightStar Care in Delray Beach, Florida, told WPBF News. “From the beginning, home health has kind of fallen into this blind spot.”
More than half of the respondents in HHCN’s vaccine survey said their state had explicitly prioritized both home health and home care workers in their prioritization strategies. About one-quarter said their states didn’t prioritize any in-home care workers.
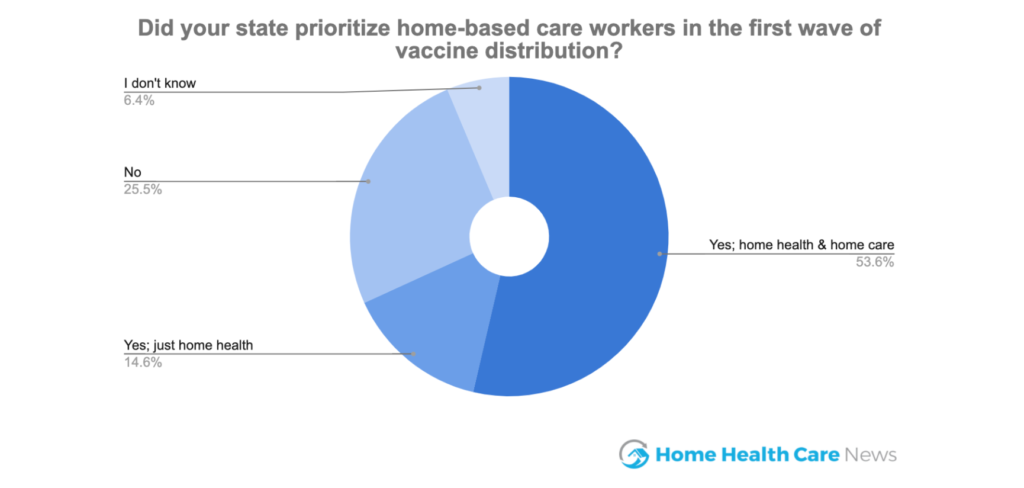
Los Angeles County in California is the epicenter of the pandemic right now. Its local government did clearly confirm home health and home care workers are eligible for the vaccine.
After initial confusion, Colorado officials announced on Jan. 19 that individuals who provide in-home health care for homebound elderly or sick people do qualify to receive the coronavirus vaccine in the current distribution phase. Massachusetts opened up eligibility to all in-home health care workers last week, too.
Considering the “Herculean” vaccine undertaking, Anderson told HHCN that difficulties with the “sausage-making process” were to be expected.
“But there are good stories, too,” he said. “I think Arizona has done a really nice job. At Addus, our experience in downstate Illinois has been positive. We’ve had good success with the prioritization of home care workers and their access to [the vaccine].”
‘Be Wise, Immunize’
Apart from access, home health and home care providers must also navigate vaccine hesitancy among their workforce.
In HHCN’s survey, just 10% of the respondents said their organization had a universal willingness from staff to get vaccinated. About 70% of respondents said a majority of their workforce was willing to get vaccinated.
“That’s really the No. 1 question on most people’s minds right now,” Anderson said. “It’s a bit early to tell, I think, to get a real true sense of how much vaccine hesitancy there is among this workforce.”
To help educate the in-home care workforce and alleviate anxieties, PMHC recently launched a “Be Wise, Immunize” campaign, which includes a public awareness website with information about the COVID-19 vaccine, front-line-worker testimonials, state-level guidance and more.
“We wanted to bring together facts and science-based information into one place to continue to provide education to home care workers regarding the vaccine,” Anderson said. “We really believe that the more direct-care staff hear from their peers about the positives of the vaccine, the more they get the real story about side effects, … the more we can reduce the vaccine hesitancy.”
Of the more than 100 home-based care professionals to take part in HHCN’s survey, just four said that their organization is mandating staff vaccinations. About 62% of the respondents said their organizations are encouraging or incentivizing vaccinations.
Moving forward, providers may need to start considering what they do if clients decline visits from caregivers who aren’t vaccinated.
More than two-third of the HHCN survey respondents said they are concerned about patients or clients turning away visits from unvaccinated workers.
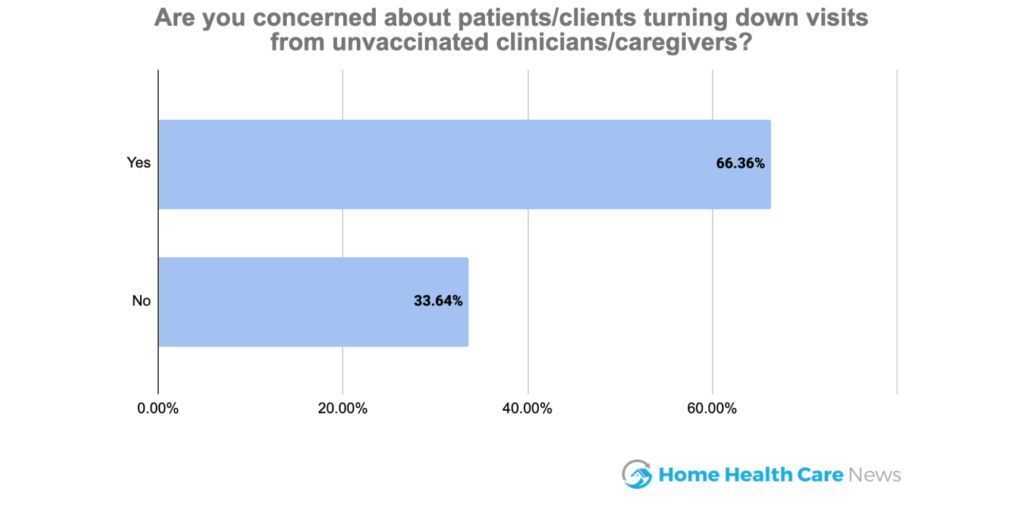
“If we get clients who say, ‘Don’t send me an aide that’s not vaccinated. Don’t send staff into my home that’s not vaccinated.’ What do you do in those situations?” Anderson said. “Nobody is really truly comfortable mandating the vaccination. But we want to encourage it — and for that very reason.”
Yet any decisions on how to encourage vaccinations depend on the nation’s stockpile. As of Sunday, it’s unclear how large that stockpile actually is.
“I can’t tell you how much vaccine we have,” Dr. Rochelle Walensky, director of the U.S. Centers for Disease Control and Prevention, told Fox News. “And if I can’t tell it to you, then I can’t tell it to the governors, and I can’t tell it to the state health officials.”
Companies featured in this article:
Addus HomeCare Corporation, Partnership for Quality Home Healthcare




