Home health agencies now have a clearer idea of what to expect from the so-called “probe and educate” process related to Medicare billing, thanks to a recently released document from the Centers for Medicare & Medicaid Services (CMS).
A final rule issued in November 2014 removed the requirement of a face-to-face encounter narrative as part of establishing a Medicare beneficiary’s home health eligibility. To “assess and promote provider understanding and compliance” with the current requirements for establishing eligibility, CMS is undertaking the probe and educate process.
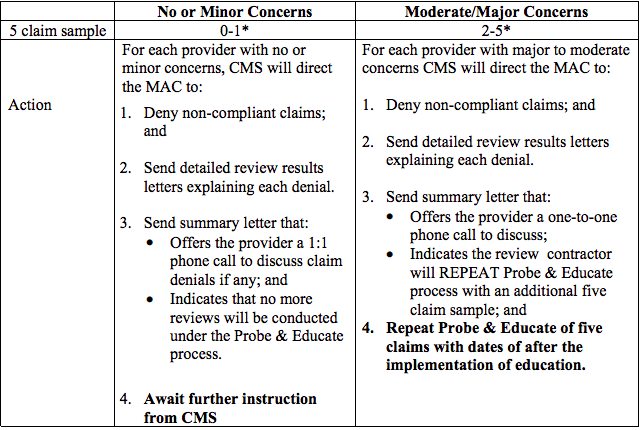
Specifically, this means that Medicare administrative contractors (MACs) will select a sample of five claims for pre-payment review for each home health agency in its jurisdiction, according to the Medicare Learning Network document. The MAC is to ascertain whether claims meet the requirements for coverage and payment, including the rules around establishing beneficiary eligibility, such as through the certifying physician incorporating medical record information in the documentation and signing and dating it.
Each non-compliant claim will be denied, and the MAC will send a letter of explanation to the agency and also offer individual, one-on-one educational phone calls. For providers that are determined to have “moderate or major concerns,” another five claims will be sampled.
The probe and educate process is being undertaken for home health episodes that began on or after Aug. 1, 2015. The first round of reviews and education are estimated to conclude in one year.
Written by Tim Mullaney




