Editors note: This is the second column submitted to Home Health Care News from Humana Chief Medical Officer Roy A. Beveridge. A previous column, “How We Will Keep Carol at Home, Not in the Hospital” ran on Sept. 19, 2018.
By Roy A. Beveridge, MD
How do you keep seniors living with multiple chronic conditions — from diabetes to congestive heart failure — out of hospitals and in their homes where they want to be?
It’s not a simple question, given the epidemic of chronic conditions we’re facing as a nation. According to the U.S. Centers for Disease Control and Prevention, approximately 75% of people over the age of 65 live with multiple chronic conditions, and 1 in 5 have an unplanned readmission to the hospital within 30 days of discharge.
Our answer
At Humana, we want to help our 3.5 million Medicare Advantage (MA) members stay in their homes and out of the hospital. We’ve invested in our integrated care delivery strategy, which specifically supports and advances the care necessary for this population.
It’s also why we finalized our agreement with Kindred at Home, which sees more than 570,000 patients daily across 40 states and is the leading provider of home health services in the country. Kindred at Home accelerates our goal to create a national care platform that extends into the home. Kindred at Home’s geographic footprint also covers approximately 65% of Humana’s membership nationwide.
Here’s how we plan to help.
A circle of acute care
Value-based care changes the model of medicine for the primary care physician (PCP) from an encounter-based relationship to one centered on the holistic care of the patient. As PCPs in value-based models take on more financial accountability for their patients’ health — meaning they are responsible for the total cost of their patients’ care — it becomes necessary for them to connect to patients outside the office.
PCPs rely on a number of relationships inherent to a value-based model — including those with pharmacists, health plans, social workers, family caregivers and many others — to extend care beyond the four walls of the exam room. It’s also important that the PCP really serve as the “quarterback” when it comes to managing the individual’s care, since the average MA member living with multiple chronic conditions has many specialists.
Care in the home becomes even more important following a patient’s hospital discharge, especially when you consider nearly every fifth hospitalization among Medicare fee-for-service beneficiaries who were discharged from the hospital alive resulted in a subsequent readmission within 30 days. We have found it’s essential to surround the value-based PCP with a circle of holistic, in-home care for their recently discharged patients within the first 24 hours of their homecoming.
This circle of holistic, in-home care is made up of six elements that depend on integrated clinical relationships inherent to the value-based care model. This 360-degree cycle of care fully supports the value-based PCP and their practice, reducing burdens to the clinician and complexity for their patients.
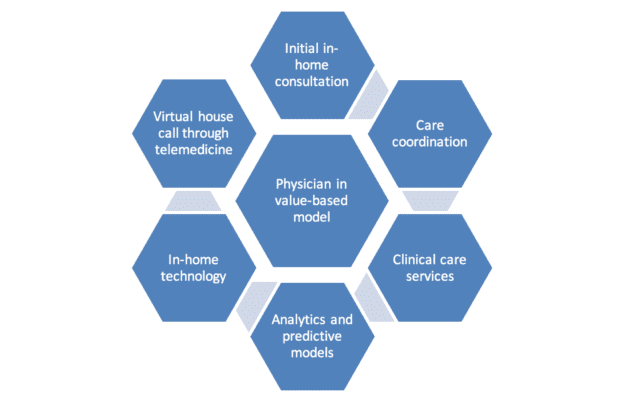
1. Post-acute first visit: A newly discharged patient is visited by a Kindred at Home nurse in the first 24 to 36 hours to immediately follow up on all current medical issues and certify a plan of care.
2. Care coordination: Thanks to data sharing capabilities between Humana and Kindred at Home, the nurse has important patient information, including diagnoses and medication reconciliation, and is able to assess and address social determinants like lack of transportation or access to good food. They coordinate care following up on medicines, appointments, and illnesses from the recent hospitalization.
3. In-home clinical care: Nurses now bring into the home clinical services such as wound care, foot exams, vaccinations, bloodwork, and efforts to promote medication adherence.
4. Analytics and predictive models: Humana is able to bolster this connected care in the home with analytical capabilities, giving physicians and their practices deeper insights into their patients’ conditions, including predictive-models that can identify those at risk for poor medication adherence and hospital readmission.
5. Always-on devices and wearables: Technology is rapidly evolving. Through Kindred at Home, integrated technology like remote digital scales and glucose monitors can alert physicians to potential patient concerns before they escalate and require hospitalization.
6. Put the physician in the home — virtually: The nurse can virtually bring the physician into the home through telemedicine to give the physician a view of their patient and the ability to immediately assess and treat.
Humana’s care coordination service has also enabled us to deliver coordinated care to nearly 1 million Humana Medicare Advantage members, and it has helped decrease hospital readmissions and hospitalizations. The integration of Kindred at Home expands on these services to bring the value-based care physician closer to the patient at home.
When we’re able to integrate these critical elements of the care circle, Humana will deliver an in-home, holistic care experience through a unified, transformative system that will help keep seniors in their homes.
In the end, seniors want to live life on their terms and the integrated care experience that Humana and Kindred at Home will deliver will transform health care.
 Dr. Roy Beveridge joined Humana in 2013 as Chief Medical Officer. He is responsible for developing and implementing Humana’s clinical strategy, with an emphasis on advancing the company’s integrated care delivery model.
Dr. Roy Beveridge joined Humana in 2013 as Chief Medical Officer. He is responsible for developing and implementing Humana’s clinical strategy, with an emphasis on advancing the company’s integrated care delivery model.
Dr. Beveridge is known for creating collaborative environments among physician communities and providing thought leadership around population health. He is a member of the Management Team, which sets the firm’s strategic direction, and reports to President and Chief Executive Officer Bruce Broussard.
Previously, Dr. Beveridge served as Chief Medical Officer for McKesson Specialty Health. Prior to McKesson’s acquisition of US Oncology in 2010, he served as the Executive Vice President and Medical Director at US Oncology. He has published extensively in the fields of medical oncology, stem cell transplantation, quality design and population health.