Home health care is becoming well known for its ability to help reduce rehospitalizations and lower overall health costs. But some high-risk patients are still in danger of a readmission even after a home health discharge.
As a result, some providers are working to take care of patients after an episode of home health ends, through continued coordination and interdisciplinary work. These providers and payors believe this practice could further cement the value proposition of home health care services.
Cross-continuum care
UnityPoint at Home, a hospital-based home health care provider, has been leveraging technology and data analytics to determine when high-risk patients are likely to be readmitted to the hospital. In many cases, these patients are “in the red” when it comes to their risk following a discharge from home health.
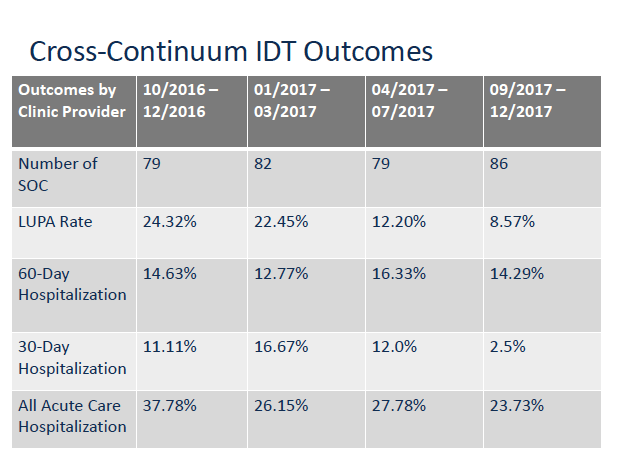
The development of an interdisciplinary team (IDT) across home heath and other clinical programs has led to better care coordination and patient hand-offs across disciplines to reduce hospitalizations. The IDT and streamlined communication has also led to some other significant results.
UnityPoint Health (UPH) is a $4.4 billion integrated health system that operates in Iowa, Illinois and Wisconsin, and has 21 hospitals, 280 clinics, and more than 900 providers. UnityPoint at Home makes up about $380 million of the health system’s revenue, with 1,500 employees and an average daily census of 5,000 patients.
The IDT includes a home care nurse, clinical care manager, primary care physician, pharmacist, palliative care representative, and a social worker who operates both throughout the home health episode and in the physician’s office.
When a patient who is no longer considered to be homebound is being readied for discharge, UnityPoint at Home will ensure that a physician’s appointment is set up and coordinated to prevent a hospitalization and other health risks.
“It’s not a blind discharge,” Jenn Ofelt, executive director of systemwide home care at UnityPoint at Home, said at the National Leadership Conference in Washington D.C., organized by ElevatingHome and other industry associations in March. “It’s a conversation from the patient’s home to the provider [about] if they have risk coming up, but we have to discharge them because of how we are paid under Medicare rules.”
The shared social worker has become a crux of the IDT, being able to see all health and socioeconomic factors in the home and continue reviewing the patient’s status once a home health episode is over.
“That shared social worker is huge,” Ofelt said. “[He or she] is able to identify the economic needs, even if it’s just transportation…or not having access to medications. Any of those things, our social workers are able to work on, in the home care episode and in the physician’s office.”
Since being implemented, UnityPoint has helped lower overall readmissions and improve care by connecting the dots for patients even when they as a provider are limited by Medicare requirements.
“Those are the things that demonstrate our value to hospitals and physicians,” Ofelt explained. “When you start telling them things that are affecting that patient’s outcomes that they had no idea…we get the opportunity to tell the real story, and they are blown away by what we figure out when we are in the homes on what is bringing [that patient] back to the hospital.”
In addition to reducing hospitalization rates, UnityPoint at Home saw a drop in its LUPA (low utilization payment adjustment) rate over time—a surprise benefit of better communication and coordination with physicians, Ofelt said. In cases where patients were being seen just once or twice, being able to connect quickly with the physician led to more disciplines caring for the patient at home, according to Oleft.
While home health care agencies are tackling the limitations of Medicare’s homebound requirements in various ways, the trend is emerging that providers are increasingly looking to prove their value to hospitals and health systems in innovative ways when it comes to readmission rates.
Written by Amy Baxter